Combat Trauma and Psychological Impact
Understanding Combat Trauma
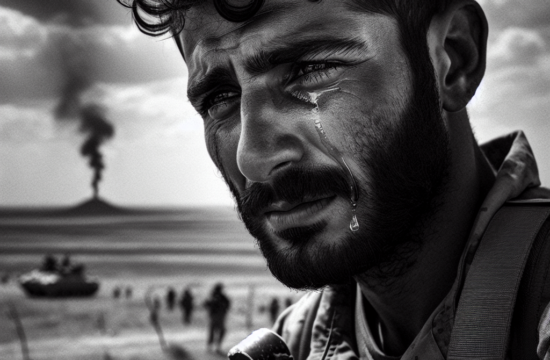
Let me tell you, the intensity of combat can leave a deep scar on a person’s psyche. Veterans often experience situations that civilians can hardly imagine. The constant threat to life, witnessing death, and sometimes causing it can build a heavy emotional burden. It’s not just the dramatic incidents that cause trauma but also the prolonged exposure to stressful environments.
==> Thank you for reading this post! Click Here If you are looking for support and Victory over PTSD.
For instance, I’ve spoken with veterans who’ve described the guilt of surviving while their comrades didn’t. This survivor’s guilt is a significant part of the trauma. The mind replays these traumatic incidents, sometimes involuntarily, leading to anxiety, nightmares, and flashbacks, which are all classic symptoms of PTSD.
Understanding the depth of combat trauma is crucial. It’s not something that fades away with time. Research shows that neural pathways change under extreme stress, making trauma a physiological issue as well as an emotional one. This shift necessitates specialized treatment beyond conventional counseling.
Psychological Impact of War
The psychological aftermath of war is no joke. Far too often, veterans come back home but part of them remains on the battlefield. This lingering presence manifests in various forms – depression being a common one. The brain’s coping mechanisms can only handle so much, and the emotional overload during combat can lead to long-term mental health issues.
I remember a buddy of mine talking about how he couldn’t enjoy anything post-service because every joy felt like a betrayal to those who didn’t make it back. This constant battle in one’s mind leads to pervasive low moods and withdrawal from social interactions, which are hallmarks of depression.
Moreover, depression isn’t just sadness; it’s a combination of hopelessness, anger, numbness, and a lack of energy or interest in previously enjoyed activities. These symptoms can be debilitating, and without proper support, many veterans struggle to reclaim their pre-service lives.
Combat Trauma Therapy
From my experience, effective therapy for combat trauma involves a multi-faceted approach. Cognitive Behavioral Therapy (CBT) is often recommended to help veterans process their experiences and develop healthier thought patterns. However, it’s not a one-size-fits-all solution.
Group therapy can be particularly effective, providing a safe space for veterans to share their experiences with others who truly understand. I’ve seen this firsthand, as bringing vets together often fosters a sense of camaraderie and reduces feelings of isolation. Hearing “I get you, man” can be incredibly therapeutic.
In addition to these, engaging in mindfulness and relaxation techniques can help. Practices like meditation, yoga, or even artistic activities provide an outlet for managing stress and reconnecting with one’s mind and body. It’s about forging new pathways to cope with the past while building a healthier future.
Reintegration Challenges Post-Service
Adjusting to Civilian Life
Transitioning back to civilian life can be jarring. The structured environment of the military is starkly different from the often chaotic civilian world. Veterans lose the camaraderie and sense of purpose they had during service, which can cause feelings of being lost or aimless.
Many veterans I know struggle with establishing a new identity. In the military, they had a defined role, mission, and community. Coming back, they often find themselves questioning their place in society. This identity crisis can contribute significantly to depression and anxiety.
Moreover, practical challenges such as finding employment, housing, and integrating into a non-military social circle add layers of stress. Reinvention is tough, and without clear guidance, many vets find themselves stuck in a limbo, escalating feelings of depression and guilt.
Family Dynamics and Reintegration
Reintegrating into family life is another major hurdle. Being away from home for extended periods generates physical and emotional distance that’s hard to bridge. Family members may fail to understand the changes the veteran has undergone, leading to strained relationships.
Communication is key here. When veterans return, their loved ones may not grasp the depth of their experiences, creating misunderstandings and frustration on both sides. I’ve seen this gap lead to significant friction, even on simple matters that would normally be resolved easily.
Therapy can facilitate better communication and understanding within families. Programs aimed at transitional support for both veterans and their families can make a significant difference. Feeling supported and understood at home lays a crucial foundation for dealing with deeper psychological issues.
Professional Reintegration Support
Professional reintegration support programs can be lifesavers. Vocational training, educational assistance, and mentorship programs help veterans transition into civilian roles that resonate with their skills and interests. The importance of these programs cannot be overstated.
I’ve seen firsthand how vital these initiatives are. For instance, mentorship programs where veterans are paired with peers who have successfully transitioned can provide guidance and hope. It’s like having a map in the fog; you still face obstacles, but you know the direction.
Moreover, job placement services tailored for veterans consider their unique skills and experiences, helping them find meaningful employment. It’s not just about landing a job; it’s about finding purpose and stability that aligns with their post-service life plans.
Stigma Surrounding Mental Health in the Military
Breaking the Stigma
One of the biggest barriers to addressing mental health issues among veterans is stigma. The military culture, which emphasizes toughness and resilience, often views seeking help as a sign of weakness. This mindset leaves many struggling in silence rather than reaching out for the help they desperately need.
Education is crucial in breaking this stigma. By fostering a culture that prioritizes mental health, we can change these harmful perceptions. Encouraging open conversations about mental health within military units can lead to early identification and treatment, making a world of difference.
I’ve seen positive changes when leaders speak openly about their mental health struggles, creating a more accepting environment where seeking help is normalized. It shows that strength isn’t just about physical capability but also about taking care of one’s mind.
The Role of Peers
Peers play a critical role in combating the stigma associated with mental health. Service members are more likely to listen to and support each other. Building peer support systems within the military can help create a more understanding and supportive environment.
Peer-to-peer programs provide a platform for veterans to share their experiences and coping strategies. This sense of solidarity can be incredibly empowering, as it validates their feelings and experiences. Knowing you’re not alone can be a crucial first step in seeking help.
Moreover, peer support networks can extend beyond active duty into civilian life, offering a continued sense of community and belonging. These networks can serve as lifelines, providing ongoing support and reducing feelings of isolation that many veterans experience post-service.
Mental Health Advocacy
Advocacy is another powerful tool in fighting stigma. Veterans who have successfully navigated their mental health challenges can become advocates, sharing their stories and encouraging others to seek help. Their voices are potent in changing perceptions both in and out of the military.
I’ve seen advocacy groups make significant strides in policy changes, pushing for better mental health resources and support systems for veterans. They bring attention to the unique struggles veterans face and the need for accessible and adequate mental health care.
Additionally, public awareness campaigns can challenge misconceptions about mental health in the military. By putting human faces to these issues, such campaigns can foster empathy and understanding among civilians, further reducing the stigma and encouraging more open discussions about mental health.
Lack of Adequate Support Systems
Identifying Gaps in Support
A major reason guilt and depression in veterans persist is the lack of adequate support systems. Often, the existing services are not sufficient to meet the complex needs of veterans. Identifying these gaps is the first step in building better support systems.
For example, mental health services for veterans are often underfunded and understaffed. Long wait times for therapy and medical appointments can discourage veterans from seeking the help they need. This delay in getting care exacerbates their mental health issues, making it harder to treat them effectively.
By pinpointing these deficiencies, we can advocate for better funding and resources. It’s about creating a holistic support system that addresses not just immediate mental health needs but also ongoing support, helping veterans navigate their post-service lives successfully.
Building Community Support
Community involvement is critical in supporting veterans. Local organizations and community groups can provide a network of care, offering various services like counseling, social activities, and peer support. These localized efforts can create a safety net for veterans.
In my experience, community support can be incredibly effective. When communities come together to support their veterans, it creates an environment of understanding and compassion. Even simple gestures like organizing veteran meet-ups or awareness events can make a big difference.
Moreover, involving the community helps bridge the civilian-military divide. It brings awareness to the unique challenges veterans face and fosters a more inclusive society. Everyone has a role to play in supporting those who have served, and active community engagement can be transformative.
Government and Policy Support
Government policies play a crucial role in shaping the support systems available to veterans. Ensuring that policies are geared towards providing comprehensive mental health care and support services is essential for addressing the root causes of guilt and depression in veterans.
Advocacy groups and stakeholders must work together to push for policy changes that prioritize veterans’ mental health. This includes adequate funding for the Department of Veterans Affairs, streamlined access to services, and implementation of specialized programs.
Additionally, continuous evaluation and adaptation of these policies are necessary to meet evolving needs. By prioritizing veterans’ mental health through robust policy support, we can create lasting changes that address the persistent issues of guilt and depression among veterans.
FAQs
1. Why is combat trauma so persistent in veterans?
Combat trauma is deeply ingrained due to the extreme stress and life-threatening situations veterans experience. These incidents can alter neural pathways, making the trauma both a psychological and physiological issue that requires specialized treatment.
2. What are some effective therapies for combat-induced PTSD?
Effective therapies include Cognitive Behavioral Therapy (CBT), group therapy, and mindfulness practices such as meditation and yoga. These approaches help veterans process their experiences and develop healthier coping mechanisms.
3. How can community support help veterans with reintegration?
Community support can provide a network of care through counseling, social activities, and peer support. It fosters a sense of understanding and compassion, bridging the civilian-military divide and offering a safety net for veterans.
4. What role does policy play in supporting veterans’ mental health?
Government policies are essential in ensuring that comprehensive mental health care and support services are available to veterans. Adequate funding, streamlined access to services, and specialized programs are crucial for addressing veterans’ mental health needs.
Original Source