Understanding Military Trauma
What is Military Trauma?
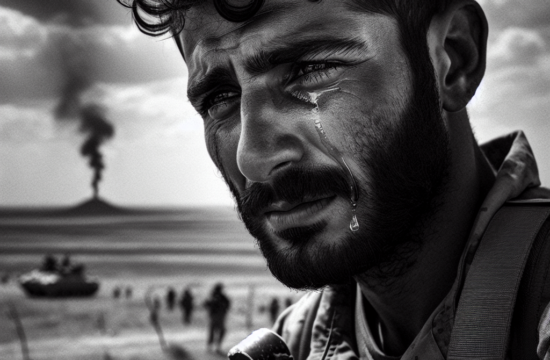
Military trauma, often associated with combat and military service, encompasses the intense emotional, psychological, and sometimes physical damage that can occur. Trust me, it’s a complex beast. Put simply, it’s not just the frontline action; it can be the stress of deployment, long assignments, or even the returning home adjustment.
==> Thank you for reading this post! Click Here If you are looking for support and Victory over PTSD.
For those of us who have been there, military trauma feels like a deeply ingrained shadow. The memories and emotions tied to these experiences can be as vivid as the day they happened. They can sneak up on you when you least expect it, often triggered by everyday occurrences.
Understanding what military trauma really is can make a world of difference in tackling it. It’s about acknowledging that it’s okay not to be okay and that seeking help is a sign of strength, not weakness.
Recognizing the Signs
One of the first steps in managing military trauma is recognizing the signs. Many people, including myself, didn’t realize they were experiencing trauma because the symptoms can be so varied. It might show up as anxiety, depression, insomnia, or even physical ailments like headaches and gastrointestinal problems.
For some of us, the symptoms can be more severe, such as flashbacks or frequent, overwhelming feelings of anger. The biggest challenge is admitting that these responses are related to our experiences in the service. It’s a tough pill to swallow, but recognizing these patterns is vital.
Talking to those who have gone through similar experiences has shown me that many of us battle the same demons. This shared understanding can form the foundation for a supportive community of fellow veterans and loved ones.
Confronting Stigma
Addressing the stigma associated with military trauma is another big hurdle. For years, there has been a stereotype that seeking mental health help is a sign of weakness. This couldn’t be further from the truth. In my view, reaching out for support shows incredible courage.
Breaking the stigma involves openly discussing mental health and the various ways trauma manifests. Sharing personal stories can significantly break down barriers and encourage others to seek help themselves. It’s about creating a culture where talking about mental health is as normal as discussing physical health.
I’ve seen that when leaders and public figures speak up about their struggles, it can make a huge difference. Knowing that someone you look up to has faced similar challenges and sought help can inspire you to do the same.
Developing a Support System
Family and Friends
Family and friends often provide the backbone of our support systems. Reaching out to those closest to you can be daunting but incredibly helpful. They can offer a listening ear, encouragement, and even help you access resources you might not have considered.
In my journey, I found that being open with my family about my struggles wasn’t easy at first. But the payoff was worth it; their understanding and support became a crucial part of my healing journey. It allowed them to better understand my actions and moods, creating a more supportive environment.
Remember, the goal is not to burden them but to foster mutual understanding. It becomes easier for everyone involved when there’s open communication. Trust in the strength of the relationships you’ve built to help you navigate these turbulent waters.
Veteran Communities
Connecting with fellow veterans can provide a significant sense of camaraderie and understanding. Veterans’ groups, either online or in-person, create spaces where members can share experiences and coping strategies freely.
During one of the hardest periods of my post-service life, joining a veteran community provided me with a safe space to express what I was going through. Hearing others’ stories validated my own experiences and gave me new perspective and strategies to cope.
These communities understand the unique challenges of military trauma and offer tailored resources and support. Whether it’s through formal groups or informal social gatherings, the veteran community is a powerful ally.
Professional Help
No support system is complete without professional help. Therapists, counselors, and mental health professionals bring expertise and tools that can significantly aid in managing trauma. Their objectivity and training can uncover underlying issues and offer targeted solutions.
Finding the right professional can take time. It’s a journey in itself, but don’t get discouraged. The connection with the therapist is often more important than their specific specialty. It’s about feeling understood and supported.
In my own experience, therapy has been a game-changer. It provided a structured environment to explore my trauma deeply and systematically, which was instrumental in my healing process. If you’re hesitant, start small but stay open to the process.
Therapeutic Approaches and Counseling
Cognitive Behavioral Therapy (CBT)
Cognitive Behavioral Therapy, or CBT, is one of the most effective therapeutic approaches for military trauma. It focuses on altering negative thought patterns and behaviors. The idea is to understand how our thoughts directly impact our emotions and actions.
My CBT sessions taught me to identify negative thoughts, challenge them, and replace them with more balanced ones. It’s like rewiring your brain, slowly but surely. This approach gave me practical tools to manage daily stressors, which was a significant relief.
CBT is structured and typically short-term, making it accessible for many. But consistency is key here. Regular sessions and practice can lead to lasting changes in how you handle anxiety and trauma-related symptoms.
Exposure Therapy
Exposure Therapy is another potent tool in coping with military trauma. It involves gradually exposing yourself to the triggers and memories of your traumatic experiences in a controlled environment. The goal is to desensitize and reduce the overwhelming fear these memories can evoke.
Initially, this sounded intimidating to me. But under the guidance of a skilled therapist, I discovered it was more manageable than I had imagined. It’s about pacing and ensuring you’re never too overwhelmed.
Over time, the things that once had a tight grip on your life start to lose their power. Exposure Therapy can be tough, but it’s incredibly freeing. It helps you reclaim control over your life, bit by bit.
Mindfulness and Meditation
Mindfulness and meditation practices provide another layer of therapeutic support. These techniques focus on staying present and acknowledging your thoughts and feelings without judgment. This can be particularly grounding for those of us dealing with trauma.
I incorporated mindfulness into my daily routine by starting with just a few minutes each morning. This simple practice helped me become more aware of my mental state and reduce overall stress. It’s amazing how such a small commitment can make a big difference over time.
If you’re new to this, apps and online resources can guide you through the initial stages. Consistency is crucial, but it doesn’t have to be perfect. Even small, mindful moments throughout the day can build resilience and calm.
Self-Care and Daily Routines
Physical Exercise
Physical exercise is a cornerstone of self-care. It has numerous benefits, from boosting your mood with endorphins to improving overall physical health. For those coping with military trauma, it’s a powerful tool that can aid recovery.
I make it a point to incorporate exercise into my routine, whether it’s a brisk walk, a gym session, or even yoga. It’s more about consistency than intensity. Over time, I’ve noticed a significant improvement in my mood and energy levels.
Let’s be real: starting can be the hardest part. But once you find an activity you enjoy, it becomes a cherished part of your day. Exercise can also be a great way to reconnect with your body and mind, providing a much-needed sense of accomplishment.
Balanced Nutrition
Balanced nutrition is equally important in managing trauma. What we put into our bodies can directly impact our mental and emotional well-being. A balanced diet can improve overall mood, energy levels, and even sleep patterns.
For me, planning meals and sticking to regular eating times made a big difference. Incorporating a variety of fruits, vegetables, lean proteins, and whole grains helps maintain a stable blood sugar level, which is crucial for mood stability.
It’s not about strict diets or cutting out all treats. It’s about balance and finding what works for you. Occasionally indulging in your favorite comfort food is completely fine. The key is maintaining overall healthy eating habits.
Sleep Hygiene
Quality sleep is essential for managing trauma. It’s during sleep that our bodies and minds truly rest and recover. Unfortunately, trauma can often lead to sleep disturbances or insomnia.
I’ve found that establishing a relaxing bedtime routine makes a huge difference. This might include activities like reading, listening to calming music, or practicing gentle stretches. It’s about creating an environment conducive to sleep.
Consistency is crucial. Going to bed and waking up at the same time each day can regulate your body’s internal clock. Avoiding caffeine and screen time before bed can also enhance sleep quality. It’s all about finding what works best for you.
Frequently Asked Questions
Q: What are some signs that someone is experiencing military trauma?
A: Signs can vary widely but often include anxiety, depression, insomnia, flashbacks, or physical issues like headaches and gastrointestinal problems. It’s important to take these symptoms seriously and seek help.
Q: How can friends and family support someone with military trauma?
A: Being open, listening, and encouraging professional help can make a big difference. It’s about providing a supportive environment where the individual feels understood and valued.
Q: What therapies are most effective for military trauma?
A: Cognitive Behavioral Therapy (CBT) and Exposure Therapy have been shown to be highly effective. Mindfulness and meditation practices can also provide significant benefits. The key is finding what works best for the individual.
Q: How important is self-care in managing military trauma?
A: Self-care is crucial. Physical exercise, balanced nutrition, and good sleep hygiene can all contribute to better mental and emotional well-being. Self-care practices should be a regular part of their routine.
Original Source